Spinal Immobilization In Deep Water
by Gerald M. Dworkin
Printed in March 1983 jems
For the past three issues, jems has presented a thorough review of spinal immobilization devices that are used in traditional rescue situations. But what about the victim who must be removed from deep water and needs spinal immobilization? The following article details the equipment and protocols for accomplishing the safe removal of such a patient.
The author, Gerald M. Dworkin, an EMT and former EMT instructor, is the Director of Safety Services for the Greater Houston Area Chapter of the American Red Cross in Houston, Texas. While he suggests coordinating training efforts with a local Red Cross chapter, the recommendations and information provided in this article are those of the author and may not reflect the opinions of the American National Red Cross.
According to statistics released by the Regional Spinal Cord Injury Systems (Spinal Cord Injury Statistics by Young,Burns, Bowen and McCutchen), the annual incidence of spinal cord injury in the U.S. is about 52 per million population. However, only about 32 per million survive to require medical and rehabilitation services. This equates to some 7,500 new traumatic spinal cord injuries each year. Although automobile accidents account for the greatest number of spinal cord injuries, sports and recreational injuries account for the second leading cause. Water-related injuries are considered to be the major cause of recreational or sports related spinal cord injuries.
Spinal cord injury occurs predominately in young people, with the average age at onset for all cases at 28.7 years. Fifty percent of the injuries affected individuals below 25 years. The most common age is 19. Almost half of the injuries occurred in the 15 to 24 year age group. Males account for 82 percent of all spinal cord injuries.
The highest incidence of spinal cord injuries occurs in July, with the lowest in January and February. A steady rise occurs in the spring months and a decline in the fall months. Saturdays and Sundays are by far the high risk days. This information presents a possible correlation between the incidence of spinal cord injuries with the involvement of recreational or sports activities, and in particular, water related activities.
Diving injuries are a major cause of spinal cord injury. They are characterized by a high percentage of complete quadriplegics. Most result from horse play and poor judgment, and about half occur in rivers, lakes and oceans where proper immobilization and removal procedures are extremely difficult.
Of the spinal cord injuries occurring in swimming pools, many happen at the home. The potential for this type of accident increases each year with the increasing number of backyard pools. Most are built with fairly low depths and usually come with slides, diving boards, or diving platforms. Spinal cord injuries in swimming pools are normally caused by any one of the following four activities:
- Diving too deep off the diving board and striking the bottom before leveling off.
- Diving or sliding too far out off the board or slide and hitting the bottom incline.
- Diving into shallow water from theside.
- Striking an object underwater (i.e.side of pool, another swimmer, etc.).
Handling Patients in Shallow Water
If the victim is found in a prone position (face down) in the water, he should be carefully rotated to a supine position (face up). To do this, the rescuer must be careful to avoid any bending or twisting of the patient’s neck and torso. The rescuer places one hand along the midline of the patient’s back at the approximate level of the armpits while the other hand is placed on the patient’s upper arm, close to his armpit. The rescuer then rotates him by lifting his arm up and over while maintaining proper head and body alignment with the other hand. To assist in getting the patient into a horizontal position in the water before the rotation, the rescuer should slowly walk back with his hands in position on the patient. This technique helps to align the entire body prior to rotation.
Once the patient is in a supine position, the rescuer should then move alongside, continuing to support the victim with one hand behind his neck and the other along his back. This maintains proper alignment and keeps the patient horizontal. Additional rescuers should bring the necessary equipment, and a cervical collar should be positioned around the patient’s neck.
To place a backboard under the patient, rescuers should position themselves at each end of the board, which is floated alongside the patient in the water. On command, the rescuers lower the board beneath the patient and allow it to come up slowly to support him. Care must be taken during the ascent of the board to properly align it with the patient. The original rescuer is responsible for supporting the patient and maintaining his alignment in a supine position until this is accomplished. Once the board is in place and the patient is adequately resting on the board, the original rescuer may then begin immobilizing him.
Sandbags are placed along both sides of the patient’s head in order to reduce the risk of any lateral movement. Once this is accomplished, the immobilization of the patient to the board may begin. The author recommends the following sequence of securing the patient to the backboard:
- Across the chest, under the armpits.
- Above the waist to include the arms at the sides.
- At hips to include hands at sides.
- Above knees.
- Above the ankles.
- Across the forehead.
This technique allows for the greatest mass of the body to be secured before the head. This reduces the chance of the head being hung up on the board should the body move due to wave action.
If the injury were to occur in deepwater, the rescuer should approach and rotate the patient in the same manner as in shallow water. However, the rescuer must be a strong swimmer or wear a personal flotation device (PFD). The backboard should be placed under the patient by available rescuers and the patient should then be floated to shallow water. Again, this is a very complicated skill and can only be accomplished by skilled swimmers or rescuers wearing PFDs. If the placement of the backboard in deep water is not possible, then the patient should be floated to shallow water.
The Flotation Basket Stretcher
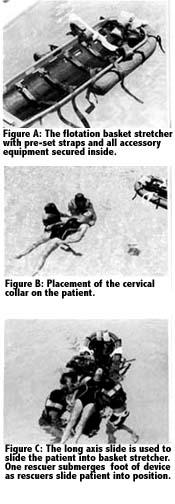
This device is recommended for deep water use when on shallow water is available. It is a standard basket stretcher with a full-length rigid backboard secured inside (Figure A). A tiedown at the head and foot of the backboard, securing the backboard to the basket stretcher, should be sufficient for this purpose. A foam-filled flotation collar, or some other type of flotation device, is attached to the outside head and shoulder section of the basket stretcher to provide sufficient bouyancy for the device, the patient and two rescuers. Flotation is only attached to the head and shoulder section of the device so that the foot section can be submerged underwater, below the patient. Several holes should be drilled through the bottom of thebasket stretcher in order to allow forwater to drain when the device is removed from the water. As with all spinal immobilization devices, sandbags, a cervical collar, and sufficient immobilization material (straps, bandages, etc.) must be available in order to properly immobilize the patient to the backboard within the basket stretcher.
Areas for Use
The flotation basket stretcher is recommended for use at any location where shallow water is not accessible and, due to the nature of the activity, the potential for injury exists. Constant depth pools (water polo pools, diving well, etc.) or other pools where the shallow end is separated from the deep end by a bulkhead are only a few examples of where this device could be kept ready for use. Marine vessels (police and fire boats, Coast Guard and Coast Guard Auxiliary) should also be equipped with this type of device for handling spinal injuries resulting from collisions, water skiing accidents, etc. Guarded surf beaches would also benefit from this device.
Sports or recreational activities that take place in the water and create the potential for this type of injury include: wind surfing, body surfing, board surfing, water skiing, springboard and platform diving, jet ski and jet bike recreation and competition, power boat racing.
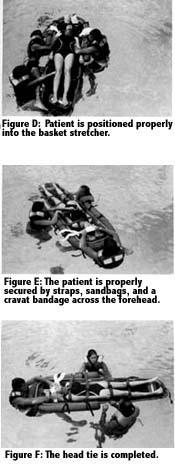
The placement of the flotation basket stretcher under a patient in deep water requires the use of two to three rescuers. Rescuer #1 rotates the patient to, or maintains the patient in, a horizontal and supine position. Rescuer #2 places a cervical collar around the patient’s neck while Rescuer #3 positions the basket stretcher in preparation for placement under him (Figure B). The foot of the basket stretcher (the end without flotation) is placed at the patient’s head. Rescuers #2 and #3 grab the patient’s upper arm in close proximity to the armpit, and slide him up the board while Rescuer #1 submerges the board beneath him (Figures C & D). Because the foot of the basket stretcher has no flotation attached, it can be easily submerged for this purpose. The support provided by the water as well as the flotation inherent in the device itself provides sufficient support for the entire body.
Once the patient has been placed appropriately on the board within the basket, the head would be sandbagged and the straps secured properly for immobilization (Figures E & F). Regardless of what type of securing system is used (bandages, velcro straps, quick release buckle straps, etc.) care must be taken to assure that the patient is secured to the backboard only and not to the basket stretcher. Once the patient is secured as already described, the head should then be immobilized to the board with cravat bandages.
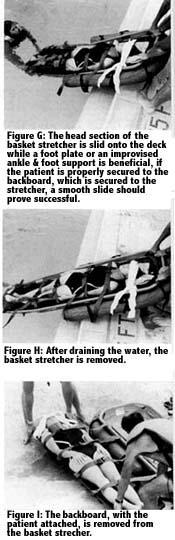
Now secured, the patient should be floated along the long axis of the body to the platform (dock, pool side, shore, boat, etc.) for removal from the water. The head of the basket stretcher can be pulled onto the platform while the foot of the basket is allowed to drop deeper into the water (Figures G & H). This will also allow water to drain from the basket stretcher. After removal of the basket stretcher from the water, the two straps securing the backboard to the basket stretcher can be removed so that the backboard, with the patient secured on it, can be removed from the basket stretcher (Figure I). With the patient adequately secured to the backboard,and the board free from the basket stretcher, the patient can then be transported to the medical facility.
Other Uses
In addition to aquatic-typeemergencies, the basket stretcher is recommended for any situation involving the movement of a patient over rough terrain or lifting, turning or extended carrying of the patient. Ambulance and rescue personnel faced with the problem of moving a patient in cardiac arrest down a flight of stairs while maintaining CPR can also use the basket stretcher for this purpose. The construction and design of this device makes it the most practical available. Handholds are built in, and the devicei tself provides a rigid support for the patient. A patient properly immobilized within the basket stretcher can be placed vertically, turned on his side,and slid downstairs if necessary.
However, once a patient is placed within the device, it is extremely difficult to remove him unless previous provisions have been made. It is recommended that a blanket or backboard be placed within the basket stretcher before the patient, or that the patient is placed within the basket stretcher by the use of the blanket or backboard, depending upon the extent of the injuries. The author recommends the use of the basket stretcher on all ambulances for patient handling purposes.
Recommendations
The standard basket stretcher has many practical uses in the EMS field. With a backboard secured within the basket stretcher and a flotation collar attached to it, the stretcher can prove to be a very effective device for the immobilization and removal of spinal cord injured victims in deep water.
All aquatic facilities should be equipped with backboards for the handling of spinal cord injuries. If the facility is designed in such a way that the deep water is physically separated from the shallow, provisions must be made for the proper handling of spinal injuries when no shallow water is available. In addition, all organized agencies conducting aquatic activities with the potential for traumatic accidents should be prepared to properly handle this type of emergency without aggravating the injuries while immobilizing and removing the patient from the water. The use of the flotation basket stretcher allows for the immobilization and removal of the spinal cord injured victim who is in deepwater.
Because of the incidence of injuries and drowning in this country associated with aquatic type activities, it is the recommendation of the author that all EMS training include the handling of aquatic emergencies. One course already in existence is the American Red Cross Advanced First Aid course, which includes a practical unit in the instruction of elementary rescue techniques (non-swimming rescues) as well as instruction on the handling of spinal cord injuries in the water. In addition, the Red Cross provides training in lifesaving and water safety through a variety of lifesaving, swimming and aquatic survival courses. One course of special interest is Basic Water Safety which includes information on elementary rescue techniques, the handling of spinal cord injuries in the water, artificial resuscitation, and boating safety and rescue skills. This is a certified course and requires approximately four hours of instructional time. Students enrolled in this course are not required to have any swimming skill as a prerequisite as all skills are practiced in shallow water. It is the recommendation of the author that all EMT training courses include this course within their curriculums. However, any curriculum can be developed to meet these training needs. EMT coordinators should work with their local Red Cross chapters in planning this type of training program for their students.


